Innovation
Using digital tools in a deprived COPD patient population to improve outcomes
Competition
Competition 21 - Phase 3, Real-world Implementation: Respiratory Diseases and Cardiovascular Diseases
Linkedin: /companylenus-health
Project Lead
Marcia Rankin-Smith, Digital Consultancy Lead

In the UK, approximately 3m people live with Chronic Obstructive Pulmonary Disease (COPD), with a further 2 million estimated to be undiagnosed. There are over 100,000 COPD-related hospital admissions, costing the NHS more than £675m annually. Moreover, deprivation in patients with COPD is associated with increased emergency health care use, health care costs, and mortality.
Hull has a high rate of social deprivation with the city ranking fifth in England for the index of multiple deprivation (IMD). The prevalence of COPD in Hull and East Yorkshire and the rate of emergency hospital admission for COPD are both nearly double the national average.
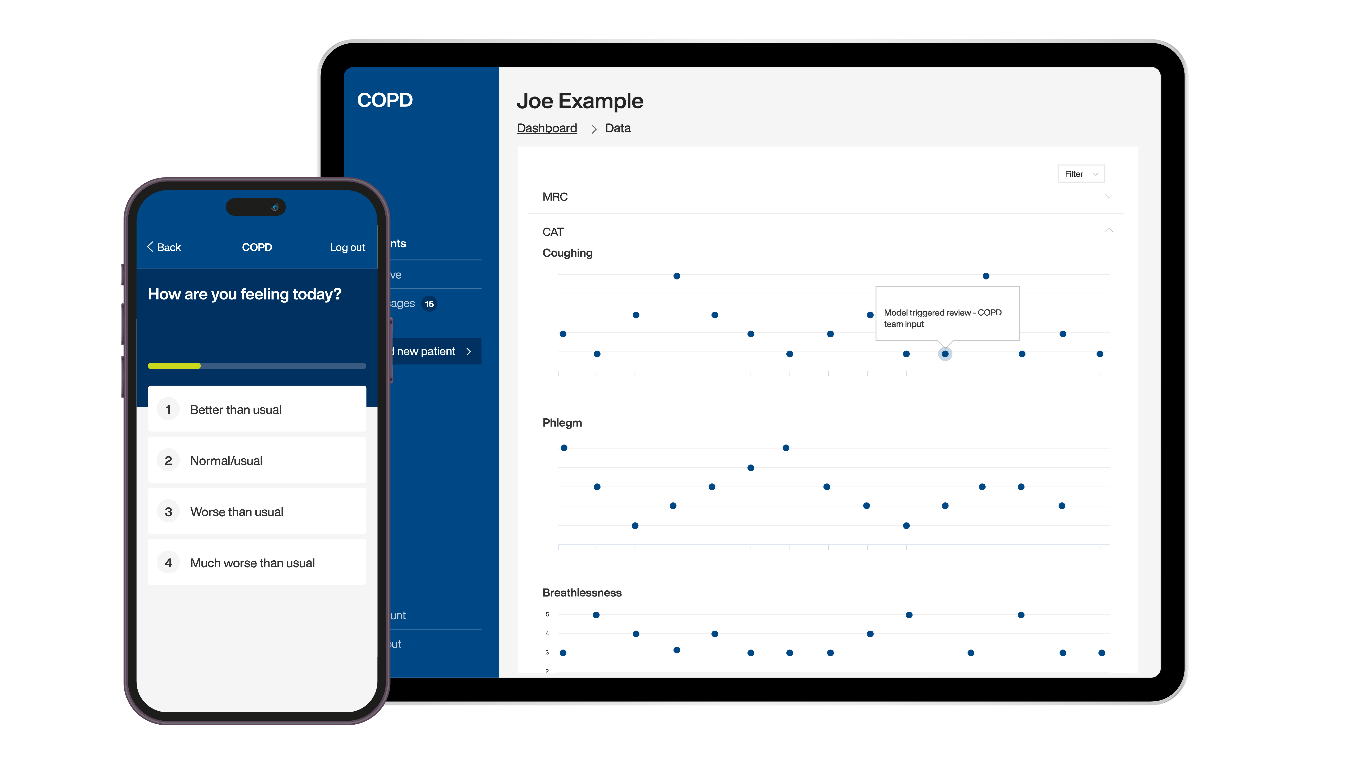
The SBRI Healthcare project enabled the implementation, economic and clinical evaluation of digital tools (Lenus Treat) on a supported self-management pathway for COPD throughout Hull University Teaching Hospitals NHS Trust (HUTH).
Interim results from the DYNAMIC-ROSE study found lower emergency department attendance rates (32% vs. 50%) and hospital admission rates (16% vs. 31%) compared to historiccontrols. In addition, an independent early economic model was generated from the costs and benefits of the service, which found Lenus Treat both less costly and more effective than standard of care over the evaluated window, including evidencing in-year savings to be achievable even with a small patient cohort.
The compelling clinical and economic evidence generated from this innovative SBRI Healthcare project paves the way for transforming the delivery of COPD care through digitally supported self-management and shared decision-making and highlights the significant potential of digital tools to improve health outcomes in deprived COPD patient populations.
Patient and public involvement and engagement (PPIE) played a crucial role in the project, ensuring real-world relevance of study design especially in relation to equity in access across deprivation demographics.
“One of the characteristics of COPD are periods of worsening symptoms, called exacerbations. COPD exacerbations are a common reason for hospital attendance, admission and negatively affect sufferers' quality of life. The DYNAMIC-ROSE study has provided early additional evidence, that builds on the work in Glasgow, that Lenus’s digital service can help to reduce the frequency of COPD exacerbations that require hospital treatment and admission. This has great potential to maintain patients’ wellbeing and also free-up valuable hospital resources.’’
Prof Michael Crooks, Respiratory Consultant, HUTH
Impact
-
Inclusion in NICE EVA draft assessment of Digital technologies to support self-management of COPD
-
Leveraged further funding from Health Innovation Yorkshire and Humber and an ICB to extend the research into additional cohorts of patients
-
Contracted to accommodate up to 1,000 patients in Hull, with additional sites now using the service. Business cases related to the service are currently being developed with the ICB
-
Finalist for the Health Tech Awards “Best Health Tech Solution of the Year”
-
Significant carbon emission savings are expected based on a reduction of general ward bed days per user per year - projections to 500 Lenus Treat users would result in 85,844 kg CO2e saved
-
Prof Michael Crooks, lead investigator of DYNAMIC-ROSE, invited to present results at Respiratory Professional Care (Oct 24), BTS Winter Meeting (Nov 24) and Digital Health Rewired (Mar 25)
“Health Innovation Yorkshire & Humber has supported the governance of this project with a seat on the project steering group. Advice about further spread of Lenus’ technology has been provided, and discussions with stakeholders to discuss the applications of the technology within primary care have been brokered. As the project nears its completion, there is a plan in place to share results of the project with regional stakeholders and Health Innovation Network colleagues, through the filming of a video case study, inclusion in our annual impact report, and the hosting of a webinar to share results.”
Sophie Bates, Workstream Lead – Commercial Support and Economic Growth, Health Innovation Yorkshire & Humber
"The service is brilliant; I’ve had a flare up this week and the response was fantastic and looks to have saved me from what could have become a lengthy illness because of the swift action from members of the team. I usually worry about what winter may bring but I’m a lot more confident knowing I’ve got the support of the team at a touch of a button."
"If I need to reach out to a clinician, I know that the app is there and that I can do that. It gives you comfort and reassurance to know that it is there for you, and that you’re going to get a response."
Date published
December 2024

